It’s a busy Monday morning in ED, many ambulance are on the go. There’s been a car crash on the high street – says the nurse – we must free the rooms immediately. There is a full flow now. In a box there is a young man, the doctor observes the patient form the outside, the computer says “dyspepsia and fever”. Blood pressure, temperature, oxygen saturation, heart rate and respiratory rate are normal.
After few seconds of observing, the doctor ask the nurse to invite the patient to leave the room for the arrival of a newer patients. I think he isn’t sick, he can wait – he says.
In the last room there is an old man just transported from an assisted-living facility because of dyspnoea, fever and cough. Respiratory rates are about 25. A rapid look than the doctor orders for a rapid admission in a non intensive care unit.
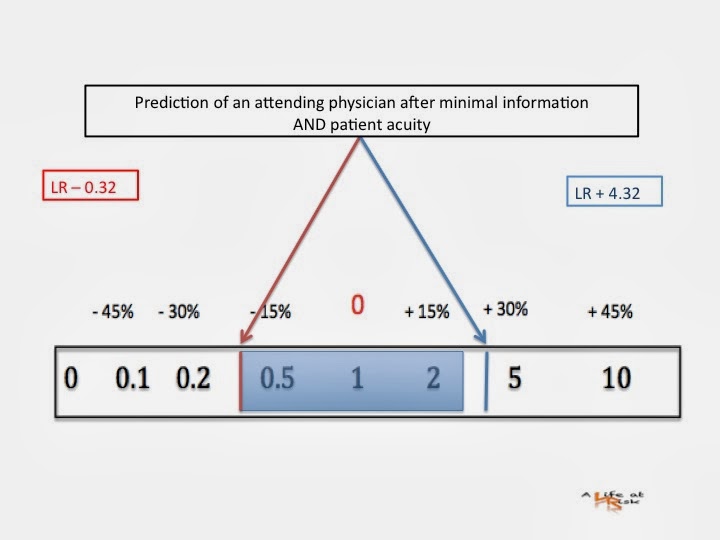
How reliable is the first look?
Conclusion
Everyday emergency physician makes an incredible number of clinical decision. Speed, synthesis, acuity are necessary, on the other hand the safety of the patients is crucial. Often the decisions operate rapidly with little or no effort and automatically, (this mode of thinking is called System 1 by psychologists).
The accuracy of identify the sick patient after minimal information is limited, but the capacity of determine exactly the disposition (ICU vs nonICU) works better. Obvisiously the accuracy increases with experience.
Bibliography
J Wiswell
Sick or not sick: accuracy of System 1 diagnostic reasoning for the prediction of disposition and acuity in patients presenting to an academic ED.
Am J Emerg Med article in press (2013)
AE Elstein
Clinical problem solving and diagnostic decision making: selective review of the cognitive literature.
BMJ vol 324 23 March 2002.