It’s a routine Wednesday morning in the ED. An ambulance carries a 25 year old male patient with loss of consciousness lasted for 2–4 min, giddiness, and dimness of vision. The patient had these symptoms while he was at home, alone. The patient reports that he probably regained from his loss of consciousness after few minutes, however, although the giddiness persisted. The patient has no vomiting, involuntary movements, headache, fever, urinary incontinence, or palpitations. He refers that it he had never experienced anything similar in the past. On physical examination the tongue has a small laceration on its tip.
Was it an epileptic seizure or something else?
Conclusion
Transient loss of consciousness is a frequent cause of referral to the ED and differentiating between seizure and syncope can be challenging, especially if not witnessed. The differential diagnosis requires a careful integration of history, physical examination, and information from further diagnostic investigations.
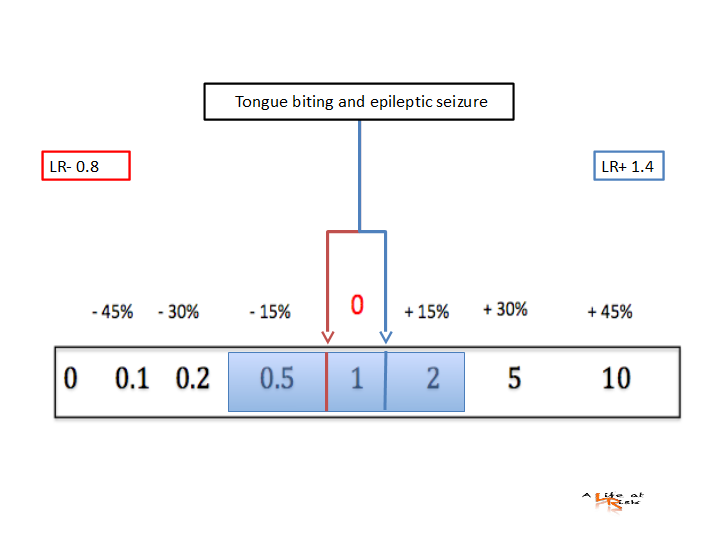
Although a tongue injury per se has no value in the differential diagnosis between epilepsy and non-epileptic events, a lateral tongue biting increases the likelihood that the patient had an epileptic seizure.
Bibliography
Tongue biting in epileptic seizures and psychogenic events. An evidence-based perspective.
F Brigo, M Storti, P Lochner.
Epilepsy & Behavior 25 (2012) 251–255 Can Assessment of the tongue on brain MRI aid differentiation of seizure from alternative causes of transient loss of consciousness?
JA Erickson, CM Benayoun, CM Lack.
American Journal of Neuroradiology June 2021, DOI: https://doi.org/10.3174/ajnr.A7188