It’s a dark night when a red code arrive at the ED by ambulance.
Paramedics tell you: “called for acute dyspnoea, I think it’s a COPD exacerbation, he is wheezing, I gave him bronchodilators and steroids, but he is worsening”.
He has a history of COPD and hypertension.
He presents sweaty, dyspneic, arterial pressure is high (220/110).
Physical examination is normal except for wheezing.
AP Chest X ray shows no signs of congestion.
Can you exclude an acute pulmonary oedema?
Or something else than your stethoscope and x ray is needing?
Conclusion
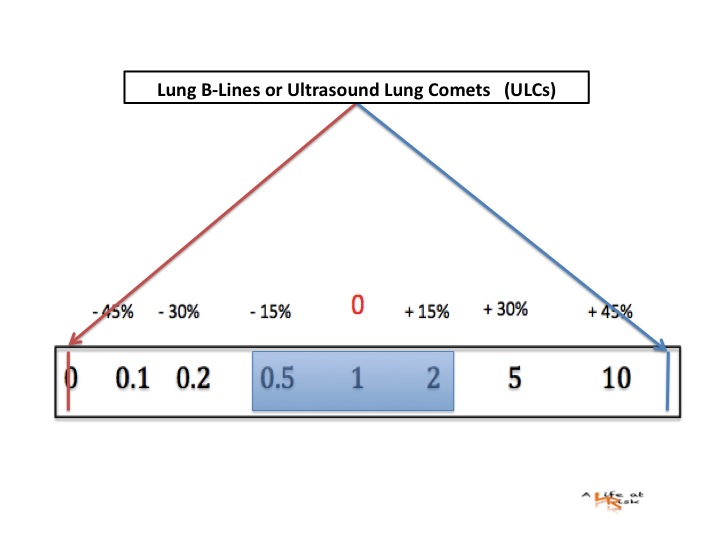
Lung ultrasond has been shown to have greater diagnostic accuracy in differentiating the causes of acute dyspnoea in emergency settings compared with the traditional methods commonly employed in emergency departments (ED).
Its major advantages, particularly over radiographic tech- niques, are the absence of ionising radiation, speed and the fact that it is unaffected by the patient’s breath-hold limita- tions or agitation.
The reliability of ULCs makes this method appealing for use in the emergency care setting. ULCs provide a direct, morphological, readily apparent imaging of abnormal increases in lung water. Recognition of diffuse interstitial involvement through B-line detection allows some pulmonary diseases to be rapidly ruled out, in particular, COPD exacerbation, which is one of the most common causes of acute dyspnoea.
Bibliography
Lichtenstein D, Mezière G (1998)
A lung ultrasound sign allowing bedside distinction between pulmonary edema and COPD: the comet tail artifact.
Intensive Care Med 24:1331–1334
L. Cardinale G. Volpicelli F. Binello G. Garofalo S.M. Priola A. Veltri C. Fava
Clinical application of lung ultrasound in patients with acute dyspnoea: differential diagnosis between cardiogenic and pulmonary causes
Radiol med (2009) 114:1053–1064
Lichtenstein DA (2007)
Ultrasound in the management of thoracic disease.
Crit Care Med 35:S250–S261