A 54 y/o man is brought to the ED because his wife has found him semiunconscious in the morning, he has not significant clincal history and does not take medicaments, he presents hypoperfused, arterial pressure is 90/50 and MAP is 63, lactate is 7 mmol/L and hemoglobin is 14 g/dl. Inferior vena cava diameter is 1,5 cm. Respiratory variation of inferior vena cava is about 25%
Conclusion
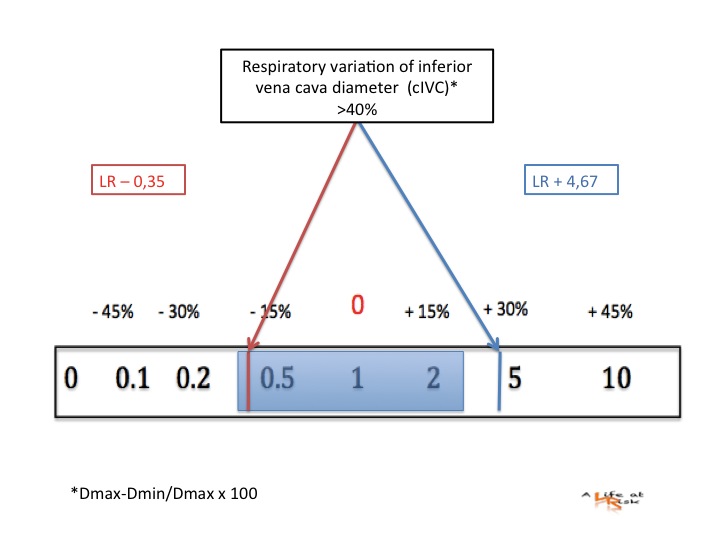
Respiratory variation of inferior vena cava is well studied in mechanically ventilated patient and it is a good predictor of fluid responsivness in this setting. Instead, in spontaneosly breathing patient there are few and small studies and it seems it doesn’t perform very well. Patient showing a respiratpry variation (cIVC) more than 40% appear to respond to fluid administration, but a less variation does not exclude fluid responsivness.
The use of passive leg raising provides a transient increment of preload.
This simple movement associated with a misure of the stroke volume variability, performed by echo at the level of aortic valve, is a good predictor of fluid responsivness in a spontaneous ventilated patient.
Those exhibiting a sustained (15 sec) increase in mean aortic flow, 30 sec after leg raising, were found to be preload responsive, on the contrary you should not fill patient that doesn’t show this improvement.
Bibliography
Critical Care December 2005 Vol 9 No 6 Pinsky and Payen
Review
Functional hemodynamic monitoring
Michael R Pinsky and Didier Payen
Marik et al. Annals of Intensive Care 2011
Hemodynamic parameters to guide fluid therapy
Paul E Marik1et al
Critical Care Research and Practice Volume 2012,
Can Transthoracic Echocardiography Be Used to Predict Fluid Responsiveness in the Critically Ill Patient? A Systematic Review
Justin C. Mandeville et al