It’s about the end of the night shift, in Observation Unit there’s George a 25 yo male presented the evening before with a mild periumbilical pain since 2 days than localized to the right lower quadrant. He was afebrile with stable vital signs, in the car, arriving to the ED, there was vomit, not diahrrea. He had a mild tenderness in RLQ. Labs evidenced WBC of 12.000 (cells/μL) and CPR of 10 (mg/L). You assessed an intermediate probability of appendicitis, than the guy remained in observation.
During the night an US of RLQ was performed, and appendix wasn’t visualized, vital signs were stable, there wasn’t vomit, a mild tenderness in RLQ was constant.
In the morning George feels better, there is no vomit, no fever, the pain is reduced. Labs returned, WBC are increased (15.000) and CPR is stable.
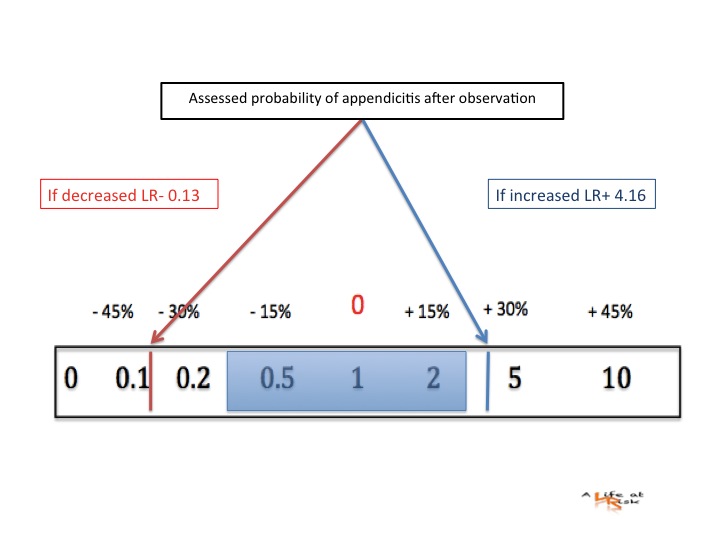
Is your assessed probability of an appendicitis changed after an active observation?
Conclusion
It was a simply non specific abdominal pain or an appendicitis that resolved spontaneously? What is important is that George feels better.
Temperature, WBC count, CPR alone have a little prediction power (see the previous post). When there is a doubt of appendicitis it is important, during the observation, to fabricate and refabricate a solid assessed probability: repeat history, revalue the abdomen, discuss with the radiologist and the surgeon, repeat exams. The change in assessed probability after observation has the best performance in avoiding false negative appendicitis.
Bibliography
RE Andersson
Repeated clinical and laboratory examinations in patients with an equivocal diagnosis of appendicitis.
W J Surg 2000; 24 479-485.
L Graff
Probability of appendicitis before and after observation.
Ann Emerg Med 1991;20:503-507.